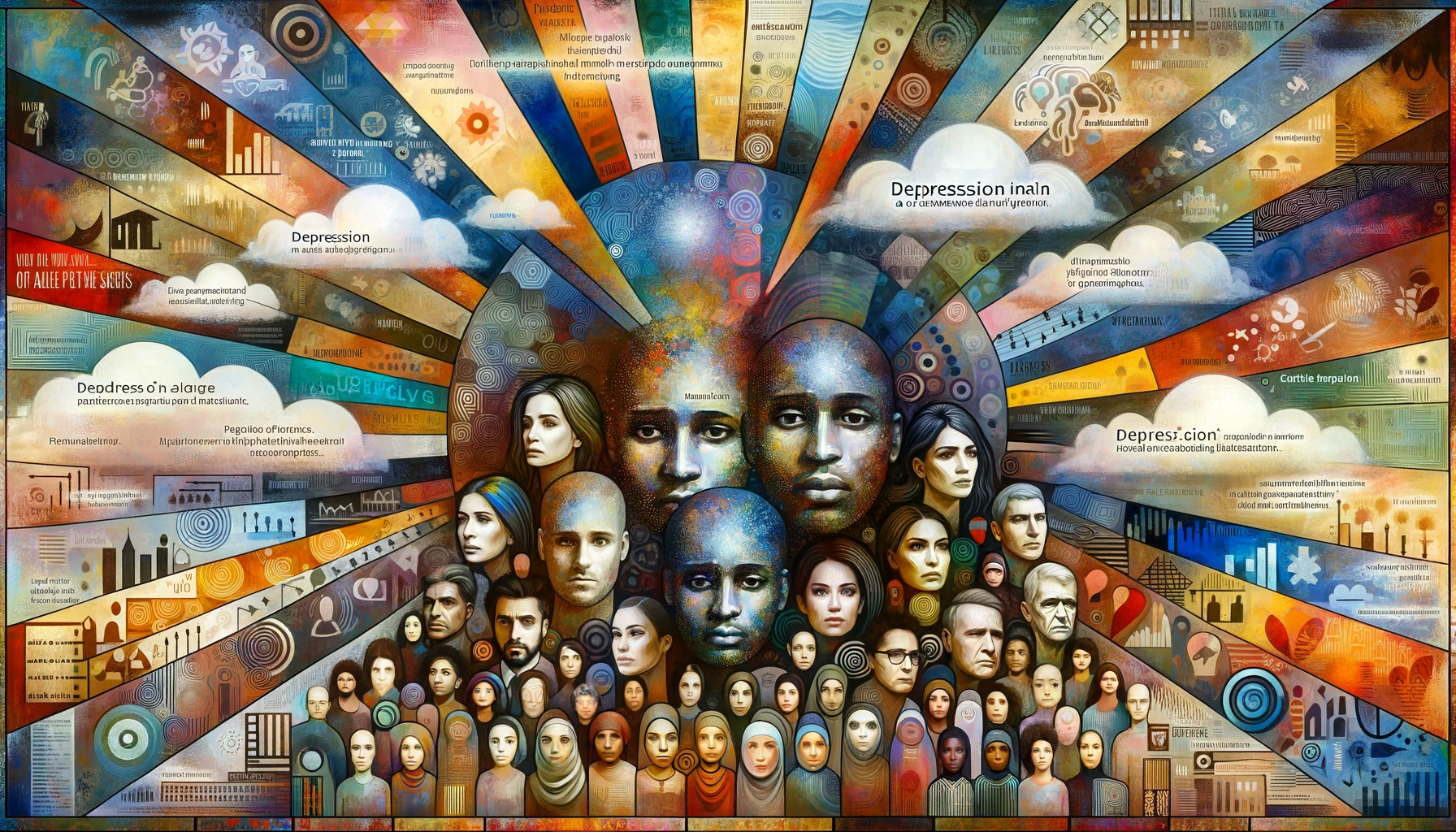
Introduction: Schizophrenia is a complex mental health condition characterized by distortions in thinking, perception, emotions, language, sense of self, and behavior. Early detection and intervention are paramount in managing schizophrenia effectively. This article explores the importance of recognizing early signs and the impact of prompt treatment in altering the course of the disorder.
Understanding Schizophrenia:
Schizophrenia typically manifests in late adolescence or early adulthood and is known for its episodes of psychosis, including hallucinations and delusions. Its early signs can be subtle and often mistaken for typical adolescent behavior, making early detection challenging but crucial.
The Importance of Early Detection:
- Minimizing Progression: Identifying schizophrenia in its early stages can significantly reduce the severity and progression of the illness.
- Improving Outcomes: Early intervention is associated with improved outcomes, better quality of life, and reduced impact on educational and vocational goals.
- Delaying or Preventing Psychosis: Timely treatment can delay or even prevent the first episode of psychosis, a critical goal in schizophrenia care.
Identifying Early Signs:
- Change in Behavior: Social withdrawal, decline in functioning, unusual behavior, or drop in grades.
- Cognitive Changes: Difficulty concentrating, following instructions, or memory problems.
- Emotional Changes: Flat affect, reduced emotional expression, or inappropriate emotions.
- Subtle Psychotic Symptoms: Odd beliefs, unusual perceptual experiences, and paranoia.
Early Intervention Strategies:
- Comprehensive Assessment: Detailed medical and psychological evaluations to rule out other conditions and confirm a diagnosis.
- Medication: Antipsychotic medications can be effective in managing symptoms of schizophrenia.
- Psychotherapy: Individual therapy, family education, and support groups can be valuable.
- Community Support: Engaging with community services for comprehensive care.
Challenges in Early Detection:
- Stigma and Denial: Individuals and families often hesitate to seek help due to the stigma associated with schizophrenia.
- Distinguishing Symptoms: Early symptoms can be vague and overlap with other mental health issues or developmental stages.
Conclusion: Early detection and intervention in schizophrenia can profoundly affect the individual’s prognosis, quality of life, and the burden on families and society. It requires a concerted effort from families, educators, health professionals, and the community to recognize early signs and provide comprehensive, compassionate care. Continued research and education are vital in improving early detection and developing innovative treatment approaches.