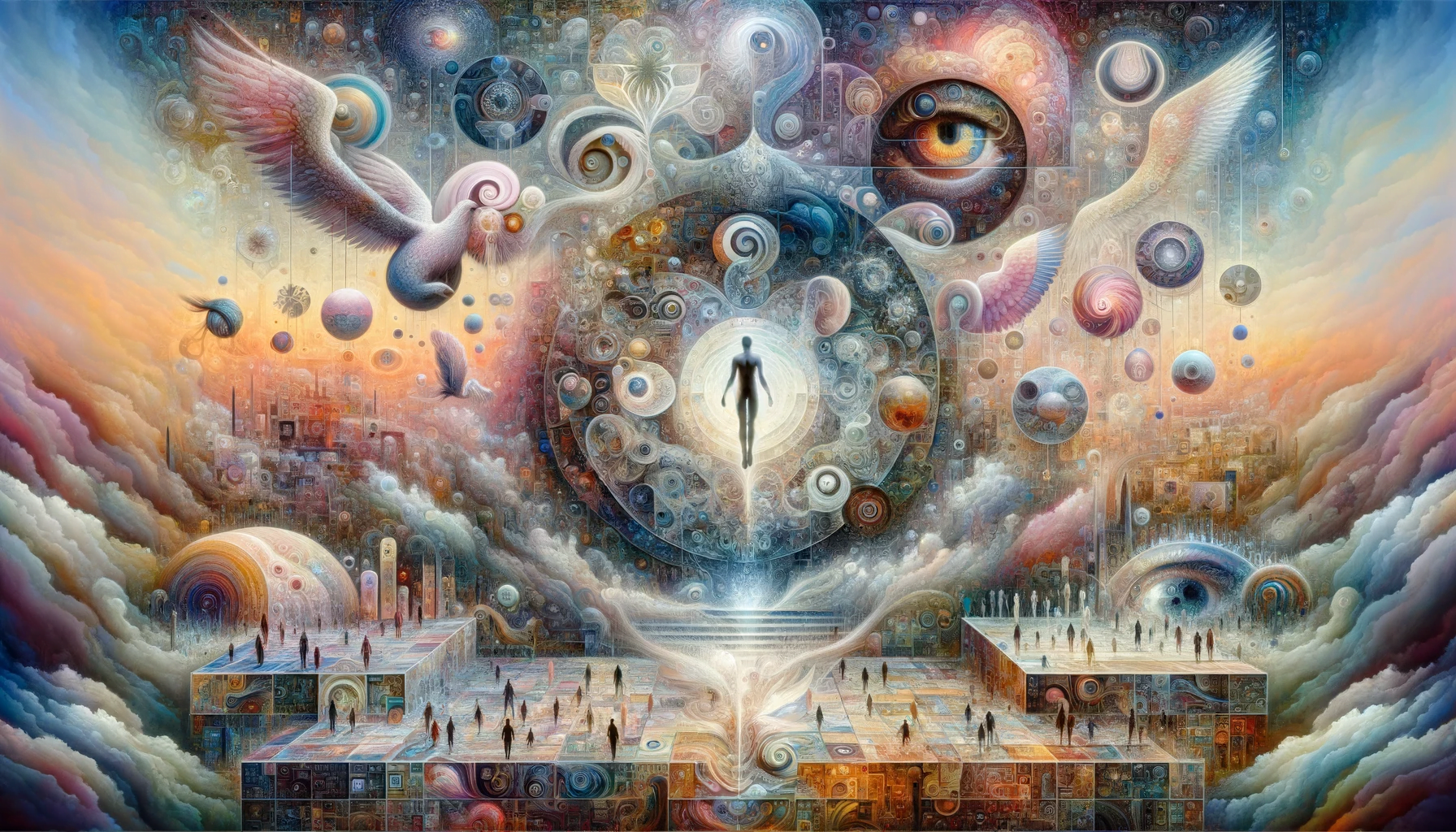
Introduction: Hallucinations and delusions are hallmark symptoms of schizophrenia, significantly impacting the patient’s perception of reality. This article provides insights into these experiences, exploring their nature, the impact on patients, and the implications for understanding and treating schizophrenia.
Understanding Schizophrenia: Schizophrenia is a chronic and severe mental disorder affecting how a person thinks, feels, and behaves. Hallucinations and delusions are among the most prominent and distressing symptoms, often leading to confusion and isolation.
Hallucinations in Schizophrenia:
- Definition: Hallucinations are sensory experiences that appear real but are created by the mind. They can affect all five senses.
- Types: The most common type in schizophrenia is auditory hallucinations, such as hearing voices that others do not hear.
- Impact on Reality: Hallucinations can be extremely vivid and convincing, leading to significant distress and difficulty distinguishing reality.
Delusions in Schizophrenia:
- Definition: Delusions are fixed and false beliefs that are not based in reality, even in the presence of clear evidence against them.
- Common Delusions: Include persecutory delusions (belief that others are out to harm them) or grandiose delusions (belief that they have special powers or importance).
- Impact on Behavior: Delusions can lead to unusual or dangerous behavior, as the individual acts in response to their false beliefs.
Patient Experience:
- Emotional Distress: Both hallucinations and delusions can cause significant fear, anxiety, and confusion.
- Social Withdrawal: Misunderstandings and stigma associated with these symptoms often lead to isolation and loneliness.
- Challenges in Communication: Explaining or discussing these experiences with others can be difficult, often leading to misunderstandings.
Treatment and Management:
- Medication: Antipsychotic medications are often used to reduce the frequency and intensity of hallucinations and delusions.
- Psychotherapy: Therapies like CBT can help patients recognize and challenge the irrational nature of their hallucinations and delusions.
- Education and Support: Educating patients and families about these symptoms can improve understanding and support.
Conclusion: Hallucinations and delusions profoundly affect individuals with schizophrenia, shaping their perception of reality and influencing their behavior. Understanding these symptoms from the patient’s perspective is crucial in providing empathetic and effective care. Through a combination of medication, therapy, and support, it is possible to manage these symptoms and improve the quality of life for those affected by schizophrenia.